Lagan Valley AC raise vital funds for CRY

The charity that helped to save the life of one of its young athletes through its screening programme June 2025 17-year-old, Scott Owen, presented a cheque for £2,000 as he shared his personal story about the benefits of heart screening in young people Lagan Valley AC has gone the extra mile, literally and figuratively, by […]
myheart hard copy newsletter-2023
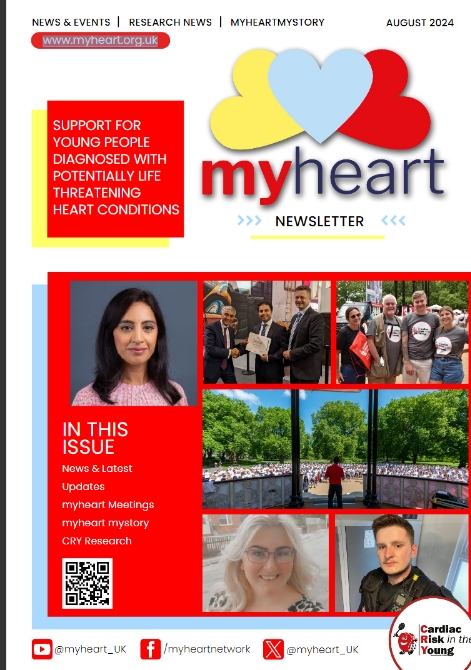
Members who subscribed to the myheart hard copy newsletter should have now received it. Read the online version here. Subscribe to myheart mailings here.
How research can lead to review and potential reform for UK screening policy

Interview with Dr Harshil Dhutia (Consultant cardiologist, Glenfield Hospital Leicester & Clinical Lead for the Inherited Cardiac Conditions service, University Hospitals of Leicester):
CRY’s Research Fellows – both past and present – are playing an increasing role in helping to inform and influence decision makers, based on their highly acclaimed, published research papers and the findings they present at UK and international conferences.
