Online myheart meeting with Dr Sabiha Gati-Saturday, 19th October, 2024
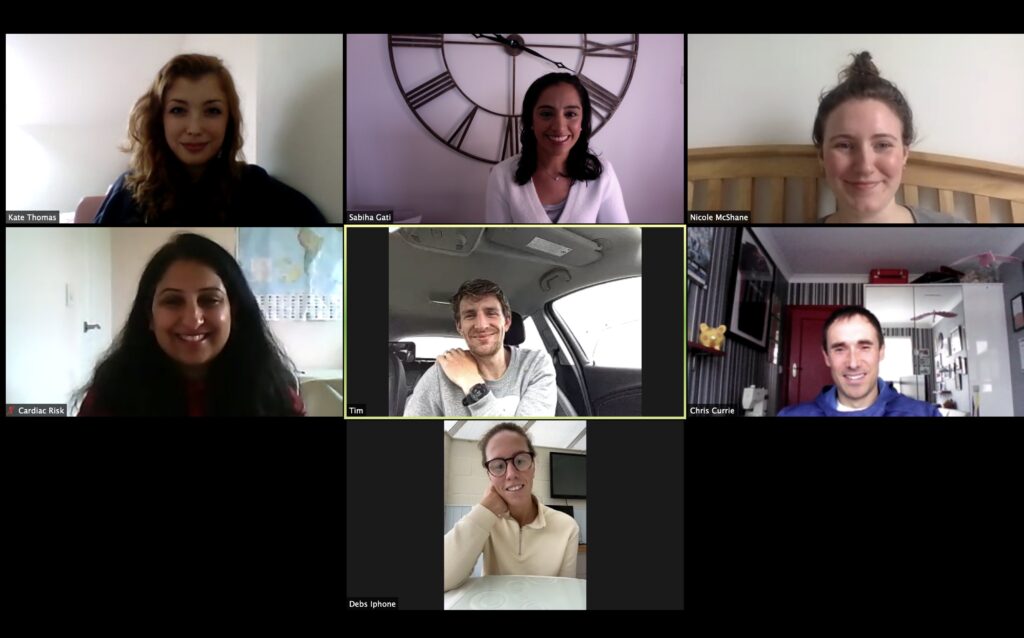
A myheart members’ video meeting is planned for Saturday, 19th October 2024 between 10am and 12pm. Meetings are free to attend and give members an opportunity to meet and discuss their experiences in an informal but supportive environment. Those young people that attend these meetings usually find them very helpful. It does not matter how long […]
myheart hard copy newsletter-2023
Members who subscribed to the myheart hard copy newsletter should have now received it. Read the online version here. Subscribe to myheart mailings here.
Never Miss a Beat

By Gem O’Reilly It’s a funny thing being told you could potentially go into cardiac arrest for something you can’t necessarily see or feel. It’s a surreal, intangible experience and very scary. That’s what happened to me when I was 16. I was diagnosed with Long QT Syndrome, which basically means my heart struggles to […]
Changes to the QTdrugs List and List of Drugs to Avoid in cLQTS

Members with cardiac conditions may like to consider registering with CredibleMeds to be kept up to date with any changes to the QT drugs to avoid list https://crediblemeds.org/everyone/. We have recently received the following message through CredibleMeds: April 29, 2024 Re: Changes to the QTdrugs List and List of Drugs to Avoid in cLQTS Dear CredibleMeds […]
National myheart meeting-16th March,2024

A myheart members’ meeting was held at Friends House, 173-177 Euston Road, London NW1 2BJ, between 2pm-5pm on Saturday 16th March 2024. Please find the feedback form below for the meeting below. There was a Q and A session with cardiologist, Dr Raghav Bhatia. In this session, members asked questions they had about their condition, the […]
Changes to the QTdrugs List and List of Drugs to Avoid in cLQTS

Members with cardiac conditions may like to consider registering with CredibleMeds to be kept up to date with any changes to the QT drugs to avoid list https://crediblemeds.org/everyone/. We have recently received the following message through CredibleMeds: December 12, 2023 Re: Changes to the QTdrugs List and List of Drugs to Avoid in cLQTS Dear CredibleMeds Registrants: […]

Leading researchers gather at St George’s University of London, to showcase a portfolio of projects funded by Cardiac Risk in the Young Friday October 20th saw the welcome return of CRY’s Annual Medical Conference to an ‘in person’ event (following three years of remote access) – with a new venue for 2023, The Curve Lecture […]
myheart hard copy newsletter-2021
Members who subscribed to the myheart hard copy newsletter should have now received it. Read the online version here. Subscribe to myheart mailings here.
CRY International Medical Conference 2021

Due to the ongoing COVID-19 pandemic, the CRY Conference was moved online again for 2021. On October 14 and 15, the conference was hosted in partnership by CRY and the European Association of Preventive Cardiology (EAPC). We were thrilled to welcome leading experts in cardiology from around the globe for presentations, discussion of case-based scenarios, […]
Atrial fibrillation
Atrial fibrillation (AF) is the most common heart rhythm disorder. It affects around 1-2% of the overall population. It is more common in men and is increasingly common as people age [1]. While it is associated with other medical conditions such as high blood pressure, obesity and other types of heart disease [2], people who are otherwise fit and healthy may still develop AF.
